In June 2012 inter-communal violence broke out in Rakhine state, Western Myanmar between the Buddhist Rakhine community and the Muslim Rohingya community, the largest stateless population in the world[1]. This violence displaced approximately 147,000 people into Internally Displacement Person (IDP) camps across the state, of which 94% were of Muslim ethnicity[2]. The Rohingya ethnic minority have since suffered from institutional discrimination, disenfranchisement from rights and services and heavy movement restrictions placed upon them, including not being able to directly access state healthcare facilities[3]. In the IDP camps of Sittwe Township[4] where the majority of the IDP camps exist, non-governmental organizations (NGOs), both national and international, collectively run static clinics to provide primary health care to the residents of the camps who cannot directly access the state health facilities.
The International Rescue Committee (IRC) has been running 22 static health clinics across 2 townships, of which 5 are in the Muslim IDP camps of Sittwe Township since 2013. This programme supports approximately 43,000 patients every year. In 2016, the team developed a Health Geo-Spatial Information Management System using a combination mobile technology and GIS software to improve programming and advocacy. By innovating the processes for better documentation of clinical consultations within the camp clinics, and enabling the data to be better analyzed, it has enabled the team to make more evidence-based decisions to improve programming. The system was developed through the combined efforts of IRC’s clinical team, Monitoring and Evaluation (M&E) Unit and Geographical Information Science (GIS) experts based in the Rakhine State.
The need to innovate
Prior to 2016, the inability to track patient history was a significant issue within the clinics, especially with the high patient volume. With some clinics receiving over 100 patients per day, the resulting record-keeping burden was substantial. Consultations were documented on paper forms and stored in-situ in the individual clinics in locked filing cabinets. Data was aggregated and reported daily to the State Health Department (SHD) in hard copy to provide real-time data for their surveillance reporting system. With the aggregations of data, the ability to track individual patient record history was therefore lost.
Another factor contributing to difficulties in patient tracking is a lack of documentation. Specifically, anyone born before 1982 may not have official civil documentation[5]. Furthermore, some of the documentation that once existed was lost in the 2012 violence when a significant number of Muslim homes and businesses were burnt down through coordinated arson attacks[6]. Subsequently, for various reasons, patients often arrive at clinics with no form of personal identification. When patients return to clinics for follow-up they may not remember the date of their last visit. Without a streamlined system of identification (i.e. no ID numbers, inconsistent spelling of names, etc.) and with reliance on a bulky paper-based filing method, it is difficult and time-consuming to locate files when looking for patient records.
From idea to impact
With an identified need for better patient history tracking, in 2016 the IRC developed and implemented the ‘Patient Consultation Booklet’ (PCB). This is a booklet distributed to all new patients visiting the clinic as of April 1st. The front cover of each PCB has a unique ID number, with no other traceable information written inside it in order to protect patient confidentiality in the event that they lose their book.
New patients at the clinics are registered by the community health workers (CHWs) before any consultation takes place (see figure 1). At the time of registration, each patient is given his or her new PCB. All data, including PCB ID number, age, gender, village/camp name and shelter location, are recorded by CHWs on a tablet with a specifically built mobile application that is saved on a password-protected database called the Patient Record Database.

Figure 1 – CHWs registering a new patient whilst recording their PCB details into a tablet with a specifically built mobile application
In the camps there is an address system that is based on the camp design by UNHCR, so it is possible to link the Patient Record Book ID to shelters, known locally as longhouses[7] (see figure 2). Each longhouse is on average home to 8-10 families. Conditions are extremely overcrowded with many of the shelters falling below emergency Sphere Standards where affected individuals should have an initial minimum covered floor area of 3.5m2 per person[8].
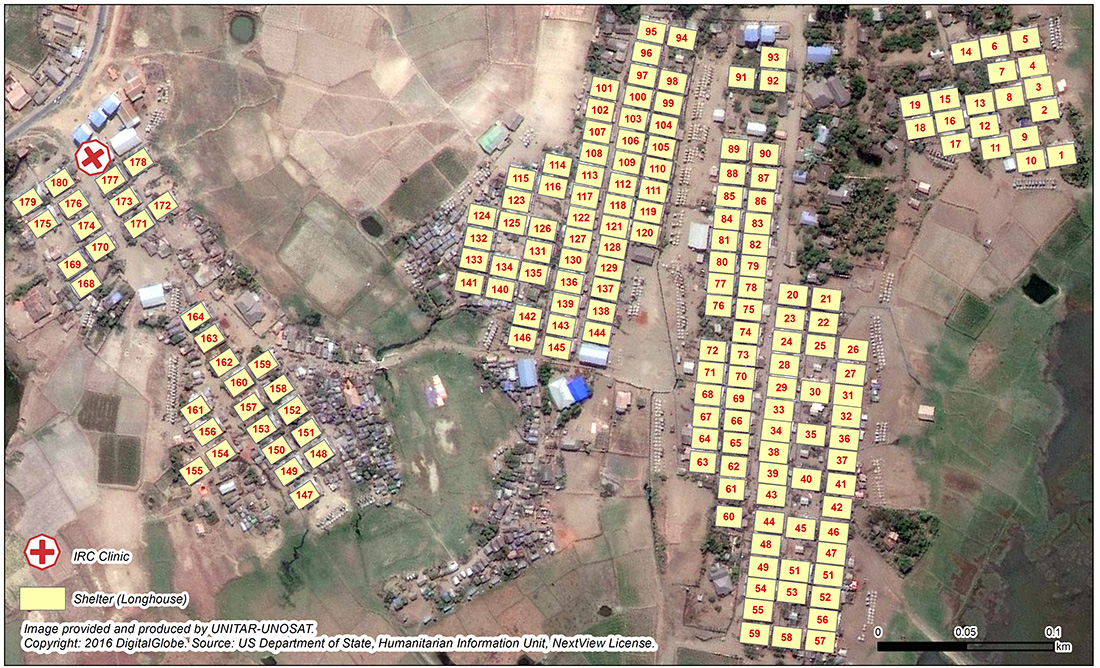
Figure 2 – Map of Dai Paine IDP Camp (Rakhine State) longhouse address system
Inside the booklet, there are carbon copy pages of the clinical consultation form, which is filled in by either a doctor or nurse during the patient consultation. Afterward, one copy of the consultation form can be removed to facilitate further follow up within the clinic (such as the prescription of necessary drugs) and then stored on location. A second carbon copy is kept within the book for the patient to take away. Each patient is asked to bring their book back for every consultation as it provides the clinical team easy access to the patient history the next time they visit the clinic. To date, this system is proving a success—since April 2016, IRC has distributed nearly 20,000 patient record books across our programme area.
The doctors and nurses in the clinics also use tablets to record the clinical information in the “Clinical Consultation Database” which is collected with a mobile application and records the same information as written on the carbon copy pages in the PCB. For every clinical consultation they record the Patient Record Book ID on the tablet version of the form, but not the patient’s name. This protects the identity of the patient but also enables a link to the location (longhouse) via the book ID, as location is recorded within in the patient record book database and can be joined via the matching ID’s in both datasets. It is then possible to join the two datasets via a relational database to which only the IRC team have access.
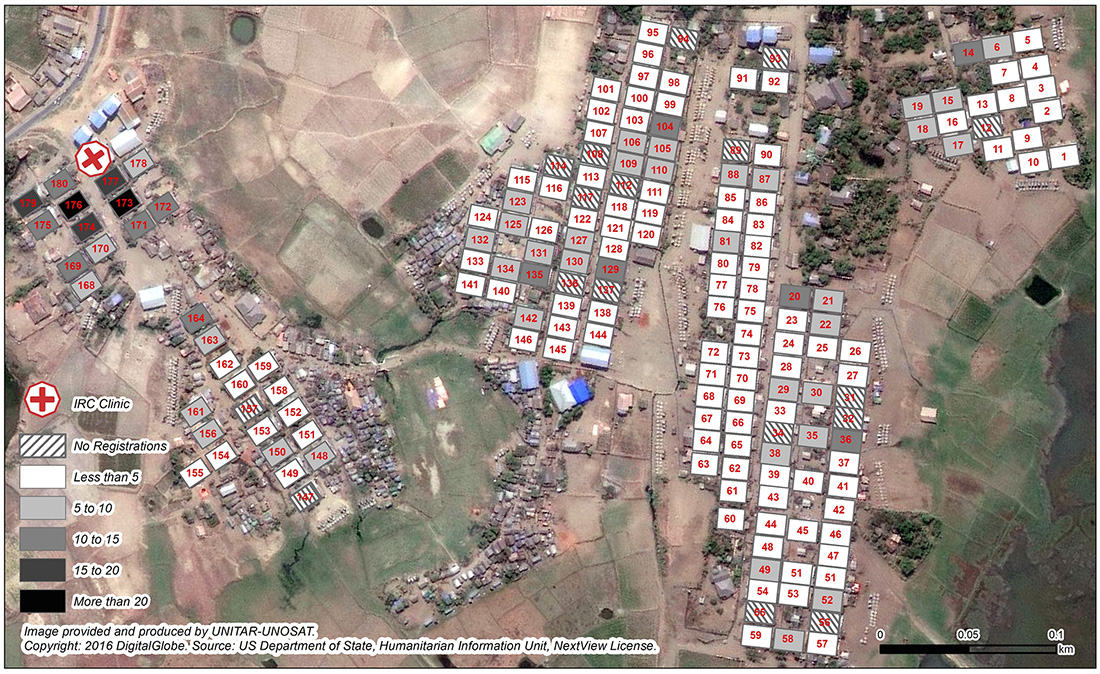
Figure 3 – Coverage of Dai Paine IDP camp clinic users per longhouse from April 1st to September 30th
Connecting clinical data to communities
The immediate outcome of this innovation was that the clinical team have direct access to patient record history via the PCB and do not lose time searching for past patient records. In addition, by recording location, it is now possible to better understand the clinics catchment areas, which has enabled the team to map both where people are coming from to access the clinic services at camp-level (see figure 3), as well as to record inter-camp movement for care-seeking behavior. It was found that a significant number of persons from villages adjacent to the camps were also the using the camp clinic facilities, which increases the clinic catchment area and thus increases the population being serviced. This has informed programming in several ways, for example by allowing the team to make adjustments in the amount of CHWs assigned per area to account for the increased catchment area[9].
This system has an additional benefit in that it provides the ability to map out common morbidities across the camps, such as diarrhea & infections, which are commonly caused by cramped living conditions. Consequently, the community health team can use these maps to inform and re-direct their health education sessions and community awareness campaigns based on where the common and preventable morbidities are coming from within the camps.
This analysis of mapping out where people are coming from in order to access health services, and what morbidities are occurring where, has helped inform how the IRC community health team work. By using clinical data, the IRC connects prevention activities in the communities to the very morbidities we are treating in our clinics. We also use the data for advocacy for shelter, WASH, and Health sector improvements in the camps with relevant humanitarian actors.
Lessons learnt
A review session was held with the clinical team and Programme Coordinator after the first 7 months of the implementation of the PCB and new health information management system. The clinical team reported that it was very useful to have immediate access to patient record history by using the PCB. It was reported that this saved time in trying to understand patient history from the patient, especially when the use of a translator was necessary in the Muslim sites[10], but also gave the clinical team better access to more technical details about previous examinations. The clinical team also reported a significant number of returning patients (post April 1st) who successfully returned to the clinic with their PCB. The clinical team overall thought this simple implementation of the PCB positively supported the consultation process and improved the quality of the health care provided.
The clinical team noted that simplification to the electronic version of the consultation form was necessary as an element of double counting was taking place, by populating the PCB and the electronic version with similar data. Completing the full consultation sheet in the PCB was deemed more critical when clinics were extremely busy as that directly informs the care being given by the clinical team at that time. For example, the nurses dispensing drugs would use the removed top page written on by the doctor to dispense the appropriate amount of drugs, whilst the data in the tablet is to inform the community health approach and more strategic programming of the project, and therefore deemed not as important during very busy periods.
The health team noted that the coding of the patient to location (either to village/camp level and also to longhouse) was very beneficial as it provided awareness of the spatial variations of access to the health clinics which has helped to better understand health seeking behaviors and blockages to health access across the different camps. Specifically for the camps, the analysis of mapping morbidities to longhouse level was less utilized due to the low statistical significance of the data being represented. The team all agreed that the continuation of aggregation of data to longhouse was the appropriate method for patient confidentiality and protection and that a shorter electronic consultation form, recording just morbidity and longhouse ID, would help provide data for targeting disease hotspots in the camps whilst not hindering the clinical team throughout the consultations
Moving forward
The team collectively agreed that continuing the use of the PCB methodology and simplifying the electronic form was deemed the best way to provide the clinical team with data to facilitate well-informed consultations, in addition to providing the community health team with data to adapt their programme to observed health seeking behaviors, blockages to health care and disease outbreaks.
As many camps around the world use address systems, such as Domiz in Iraq or Azraq in Jordan, the ability to expand this type of geospatial programming is more than possible, and not just for health, as demonstrated by UNHCR in Jordan with their innovative approach to shelter allocations in Azraq camp in Jordan. The setting up of camps are never the first option at the onset of an emergency, but when they are set up properly with formal housing structures in a structured manner, it really allows operational agencies to coordinate their response at a micro level, allowing for better tracking of aid distributions and service provision, vis-à-vis leading to a more fairer and accountable effective response. The GIS capacity within the humanitarian community has strengthened tremendously over recent years[11], therefore enabling opportunities for all different type of actors in camp environments to replicate this style of programming.
About the Author
Robert Trigwell has been working with the IRC as the Humanitarian Response Coordinator since August 2015, where he has focused on developing a data-driven response approach to programming. Prior to working for the IRC in Myanmar, Rob was the country coordinator of the REACH Initiative in South Sudan and Iraq where the team worked within the framework of the inter-agency aid coordination mechanisms developing products that enhanced the humanitarian community’s decision-making and planning capacity. Rob has a master’s degree in Geographical Information Science (GIS) from the University of Edinburgh. Rob is pursuing research into how frontline emergency responses can be better coordinated and streamlined at field level through the better use of technology.
For contact: Robert Trigwell, Humanitarian Response Coordinator [email protected] & [email protected]
Footnotes:
[1] http://fivethirtyeight.com/datalab/myanmars-rohingya-refugees-are-the-worlds-largest-group-of-stateless-people/
[2] Green, P., MacManus, T., de la Cour Venning, A. (2015). Countdown to Annihilation: Genocide in Myanmar. London, International State Crime Initiative.
[3] UNHCR Protection Analysis – Rakhine State November 2015
[4] Township is a local administrative boundary used across Myanmar
[5] 1982 Myanmar Citizenship Law sets our different categories of citizenship and grants automatic citizenship to those who are a member of the recognized 135 “national races”, which does not include the Rohingya who need to apply under different (non-automatic) provisions
[6] Green, P., MacManus, T., de la Cour Venning, A. (2015). Countdown to Annihilation: Genocide in Myanmar. London, International State Crime Initiative
[7] Distributions in the camps are often done longhouse by longhouse, so knowledge of shelter ID linked with a person or family’s name is common.
[8] Shelter & Settlement Standard 3: Covered living space – http://www.spherehandbook.org/en/shelter-and-settlement-standard-3-covered-living-space/
[9] CHW staffing ratio is 1:1,000 population:https://www.humanitarianresponse.info/en/applications/ir/indicator/h-a8
[10] The Rohingya use a different language to the ethnic Rakhine and doctors and nurses come from the Rakhine population, so commonly doctors and nurses would have to use a translator to speak to the patient
[11] An example of the GIS capacity of the humanitarian community can be seen to the extent Za’ataari Camp in Jordan has been mapped on Open Street Map (OSM): https://www.openstreetmap.org/#map=15/32.2932/36.3286

