Insecurity and COVID-19 fuel refugee mental health concerns in Libya
Insecurity and COVID-19 fuel refugee mental health concerns in Libya

Ibrahim* sits in the waiting area of a UNHCR community centre in Tripoli to see psychiatrist Dr. Hanan Al-Shremi.
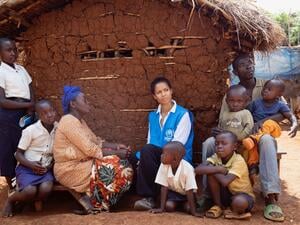
These days, Dr. Hanan Al-Shremi’s work diary is fully booked. As a psychiatrist working in the Libyan capital Tripoli, she helps refugees and asylum-seekers deal with mental health challenges such as anxiety and depression, both of which, she says, have increased significantly in the wake of COVID-19 and after last year’s security crackdown in the city.
The security sweeps in Gergaresh and other neighbourhoods created a heightened sense of fear among asylum-seekers and refugees, who are regarded by the Libyan authorities as illegal migrants, liable to arrest and detention. Many saw their shelters destroyed in the operations, leaving them homeless and worried about their safety and well-being, while thousands were put in detention.
“On average, I receive 10-12 cases a day. Previously it was five to seven cases,” says Dr. Al-Shremi, who works for the International Rescue Committee (IRC) at public health clinics and a community centre in the city run by UNHCR, the UN Refugee Agency.
“A lot come with anxiety and panic attacks. Some can’t go out to work. Physically, they are able to, but they are afraid. They feel no one is going to help them. When they come here, they feel comfortable.
"Most of them tell me ‘We… just want safety, we want to live with dignity, our ambition is not Europe’. Nobody leaves their country willingly. The most difficult thing for a person is to not have a home,” she says.
According to the World Health Organization, the COVID-19 pandemic created a global crisis for mental health, with a 25 per cent increase in cases of anxiety and depression during the first year of the pandemic.
At the same time, mental health services were severely disrupted, due to movement restrictions, making it hard for people to get the help and treatment they needed. In Libya, many asylum-seekers and refugees rely on casual labour to support themselves and their families – work that dried up as strict movement bans came into force, especially in the first year of the pandemic.
"Anxiety increased,” explains Dr. Al-Shremi. “The lockdown has had a huge [negative] impact. On some days, we were working, but people could not reach us."
Continuing treatment for her existing patients was difficult, but taking on new cases was even harder. She needed to meet them face-to-face to be able to assess their condition and provide a diagnosis and a treatment plan.

Dr. Hanan Al-Shremi consults with a pharmacist about medication prescribed for a patient.
Nowadays, there are other challenges facing those needing urgent care in Libya, Dr. Al-Shremi says. Public psychiatric hospitals will not admit refugees and asylum-seekers, while admissions to private clinics are extremely expensive. There is also a shortage of medication.
Another issue is the stigma surrounding mental health. Some patients wrongly fear it will affect their chances of being considered for resettlement or evacuation flights and ask for their files to be closed. Some discontinue treatment when they get a little better, she adds.
Despite the challenges, Dr. Al-Shremi says there are also many success stories.
"With some cases, I myself have doubts, given their circumstances. But then I get surprised when they tell me they’ve got better," she says. She mentions the case of a divorced refugee mother and her son who came for help with serious health and mental problems.
"Little by little, their conditions got better. She came to see me a week or so ago … She told me she was [being resettled] to Canada,” Dr. Al-Shremi says.
"There's no health without mental health."
Another patient is Ibrahim*, a 22-year-old who started losing his eyesight, which had a huge impact on his mental health. He has been seeing Dr. Al-Shremi for treatment for the past seven months and said the help he’d received has given him hope to continue living.
“I couldn't sleep before the treatment, thinking about my situation, feeling unsafe and not being able to see. Now I feel better,” he said.
Being able to talk more openly about mental health and getting help for those who are struggling are crucial, says Dr. Al-Shremi.
“It is so important. Distress, depression, and psychological trauma can cause destructive thoughts. Mental illness can make a person desperate, and they can lose hope,” she says.
"There’s no health without mental health.”
*Name changed for protection reasons.